Mpox Outbreak in Uganda: Reducing Stigma Through Effective Communication and Community Engagement
Mpox, formerly known as monkeypox, has re-emerged in Uganda and neighbouring countries, raising concerns about public health responses and the stigma that often accompanies such outbreaks. Understanding mpox and addressing the stigma surrounding it is key to fostering effective community engagement and ensuring timely intervention to control its spread.
Understanding Mpox
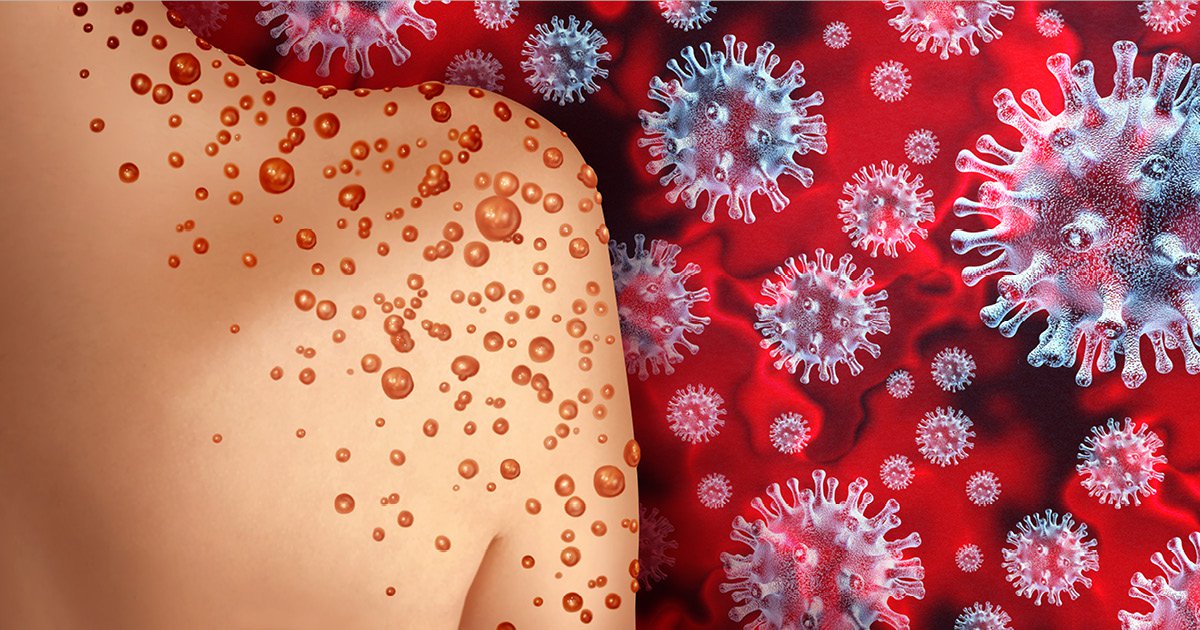
The World Health Organization (WHO) defines mpox as a zoonotic disease caused by the monkeypox virus. It primarily spreads from animals to humans but can also spread from person to person through close physical contact, respiratory droplets, or contaminated objects. In humans, the disease presents symptoms similar to smallpox, though less severe.
Key signs and symptoms include:
- Fever
- Swollen lymph nodes
- Rash that evolves into pustules and scabs
- Headaches
- Muscle aches and fatigue
Currently, Uganda is grappling with an mpox outbreak that was first confirmed in July 2024, with 11 cases reported across several districts, including Kasese, Amuru, and Mayuge(WHO | Regional Office for Africa). Surveillance systems are in place to monitor and curb further spread, but stigma remains a significant obstacle in health communication.
The Role of Stigma
Stigmatization of individuals with mpox, particularly in Uganda and other African countries, arises from misconceptions about the disease’s transmission and association with marginalized communities. The public’s unfamiliarity with mpox compounds the stigma, as many still confuse it with diseases like HIV/AIDS or smallpox.
This stigma discourages people from seeking medical attention early, leading to delayed diagnoses, continued transmission, and heightened public fear. In some communities, individuals may face isolation, ridicule, or even discrimination due to the visible rash, making it harder to reach out for help.
Effective Communication Strategies
To reduce stigma and improve mpox-related outcomes, it’s crucial to focus on the following:
- Clear, Consistent Messaging: Health authorities must provide information about mpox, focusing on transmission modes, prevention, and treatment. Messaging should emphasize that anyone can contract mpox, and it is not limited to any particular community.
- Community-Led Engagement: Involving local leaders, health workers, and community-based organizations ensures that messages are culturally relevant and reach marginalized populations. These groups can act as trusted sources of information and help dispel myths that fuel stigma.
- Media Campaigns: Leveraging radio, television, social media, and print media can amplify awareness and encourage those with symptoms to seek early treatment. These campaigns should normalize mpox as a treatable disease and promote compassion toward those affected.
- Training Healthcare Workers: Health professionals need training on how to manage mpox patients sensitively and address stigma concerns. Proper communication from medical personnel can encourage patients to follow preventive measures and receive treatment without fear of judgment.