Sanofi to launch new drug for Hemophilia A, a rare bleeding disorder
Sanofi, a French pharmaceutical company, plans to launch a new drug for a rare bleeding disorder called hemophilia A this year. The therapy, which is being developed in collaboration with Swedish drugmaker Sobi, is currently awaiting approval from the U.S. Food and Drug Administration (FDA). The FDA is expected to make a decision on the approval status by February 28th.
Hemophilia A is a genetic disorder in which the blood does not clot properly. This disorder is inherited and can affect both males and females. Symptoms can range from minor to severe, depending on the amount of clotting factor present in the blood.
Another biotech company, BioMarin, has already developed a therapy called valoctocogene roxaparvovec, which is available in Europe as Roctavian for hemophilia A. However, the therapy is still awaiting approval from the FDA.
BioMarin is hoping that new Phase III data, which is expected in early 2023, will improve its chances of getting approved. The ongoing study, GENEr8-3, by BioMarin uses a primary endpoint of change in factor VIII activity, testing valoctocogene roxaparvovec alongside corticosteroid use.
Pfizer is also developing a therapy for a less common form of the disorder called Hemophilia B. Hemophilia B is caused by deficiencies in factor IX. Pfizer plans to present additional data from the Phase III BENEGENE-2 study (NCT03861273) of its therapy, PF-06838435, in adult males with severe Hemophilia B at a scientific conference in early 2023.
Pfizer has already announced that BENEGENE-2 has achieved its primary endpoint of non-inferiority and superiority in the annualized bleeding rate (ABR), which is considered a validated marker of hemophilia activity.
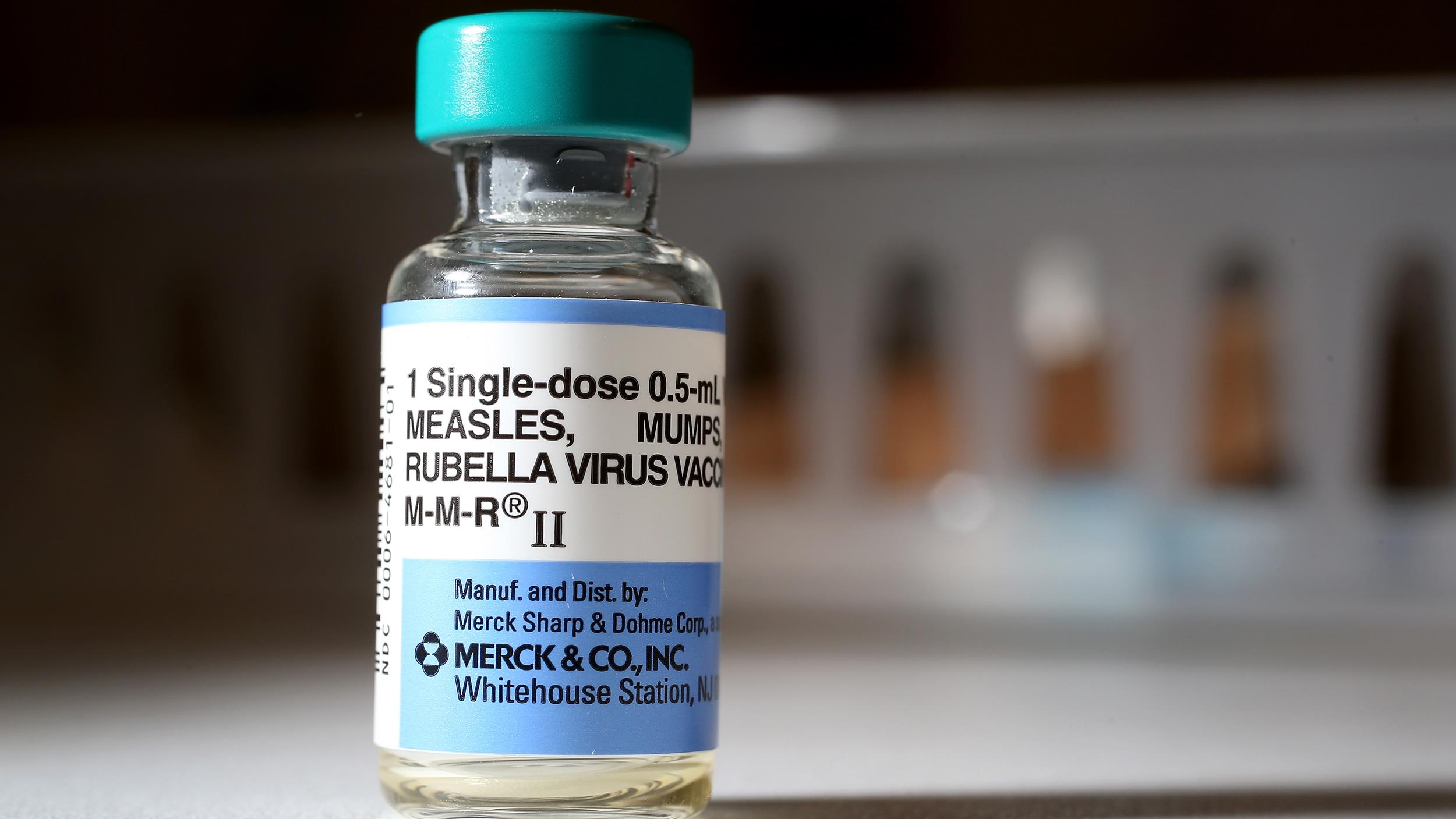
Sanofi has also followed Pfizer’s footsteps by establishing a rebate program for a blood disorder treatment called Cablivi. The program promises medical institutions a refund if inpatient treatment fails.
To qualify, patients must receive the drug in a hospital setting, and Sanofi will only cover the cost of up to six doses for those who do not respond, or up to 12 doses for those who worsen while on treatment. Cablivi became the first drug approved in the United States in 2019 for acquired thrombotic thrombocytopenic purpura (aTTP).