AFHEG Foundation and King Ceasor University Launch the AMR Club
AFHEG Foundation Joins Forces with King Ceasor University to Launch the AMR Club, Raising Awareness on Antimicrobial Resistance
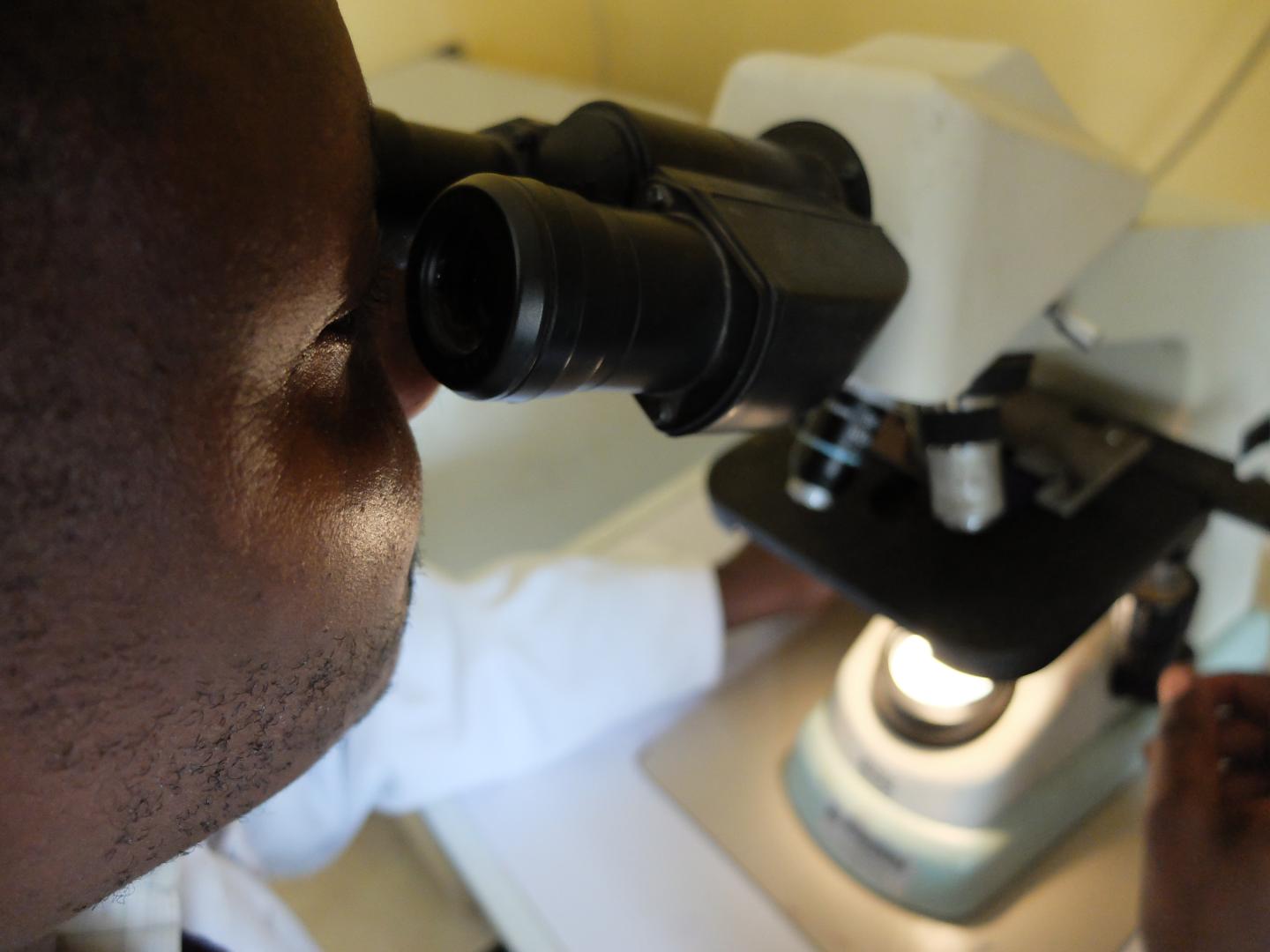
On September 14, 2024, the AFHEG Foundation joined King Ceasor University in launching its Antimicrobial Resistance (AMR) Club, marking a significant step in the university’s fight against one of the most pressing global health threats today. This collaboration emphasizes the importance of community health solutions for antimicrobial resistance and the role of education in combating AMR.

Attended by 50 medical students and lecturers, the event highlighted the power of collaboration and innovation in tackling AMR, especially within local communities. The gathering showcased the commitment of students and educators to promoting health literacy in Uganda.
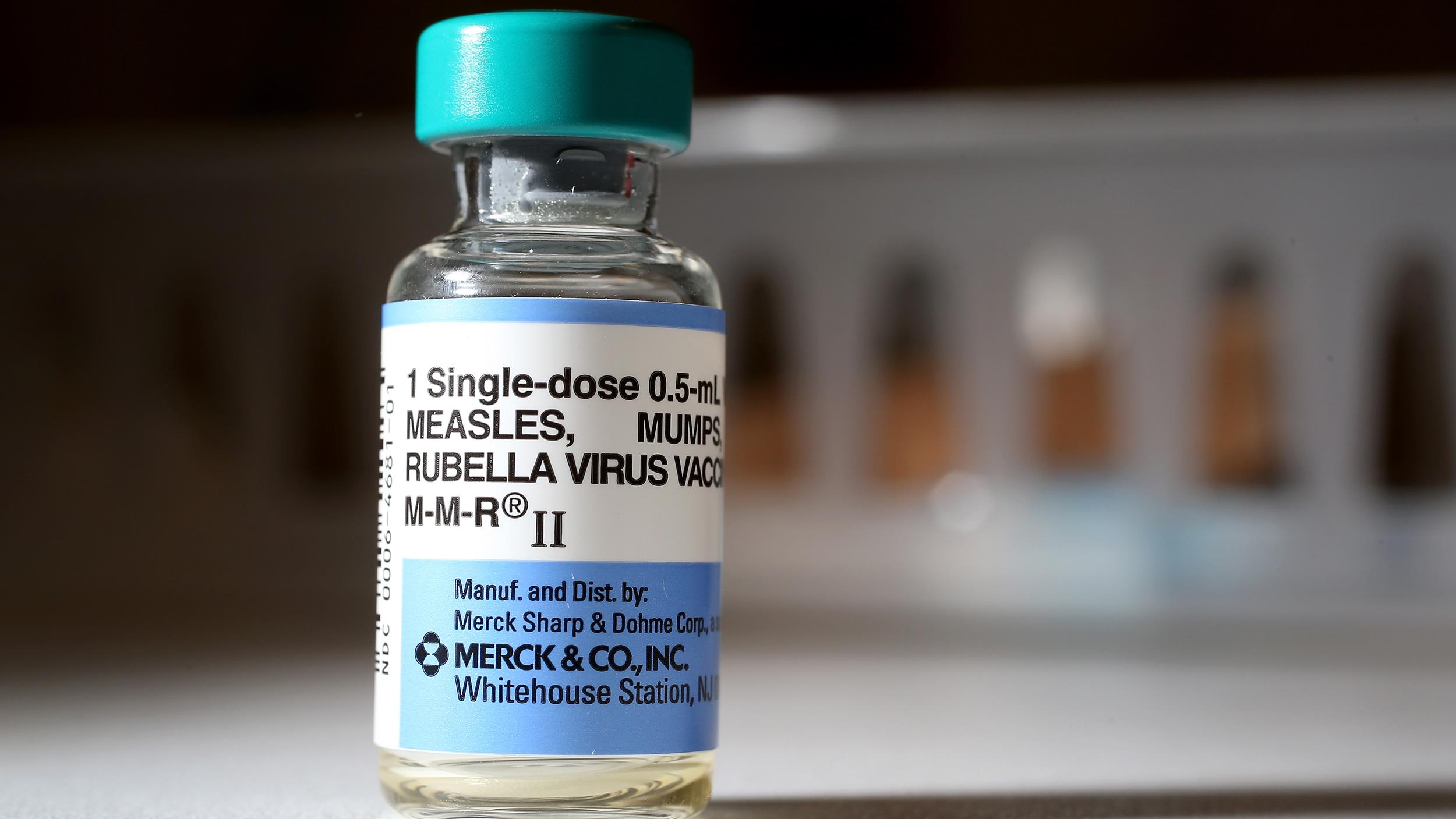
The event opened with a warm welcome from Dr. Okello Bazil, patron of the AMR Club, who emphasized the importance of following proper medical guidance. He reminded the audience to “complete the full course of medication and avoid self-medicating,” noting that adhering to prescribed treatments is essential for reducing risks like drug resistance.

Phillip Mwebaza, CEO of AFHEG Foundation, then introduced the Superbugs Clash board game, an interactive tool designed by AFHEG to raise awareness about antimicrobial resistance through gamified learning. He explained how the game educates players on the dangers of improper antibiotic use, encouraging students to share their knowledge with family and friends to foster a health-literate community. He further emphasized the transformative impact that youth-led health education can have in Uganda, where doctor-patient ratios are critically low.
The event included lively musical breaks, during which students performed songs about AMR, adding creativity to the learning experience and enhancing the impact of public health education.
Understanding Antimicrobial Resistance (AMR)
AMR occurs when bacteria, viruses, fungi, and parasites evolve and become resistant to the medicines that were once effective in treating infections. This makes common treatments like antibiotics less effective or even useless, leading to longer illnesses, higher medical costs, and increased mortality. Addressing AMR requires public awareness and strict adherence to prescribed treatments, as the AFHEG Foundation and King Ceasor University are demonstrating through education and innovative community initiatives.
Through initiatives like the AMR Club and the Superbugs Clash game, both organizations are paving the way for a healthier, informed future, underscoring the importance of collaborative efforts in health education and the need for comprehensive approaches to tackle antimicrobial resistance effectively.